When people think of weight gain, the first suspects that come to mind are calories, sedentary lifestyle, hormones, or the occasional guilt-drenched midnight snack. Rarely does one point fingers at that pear-shaped, four-inch organ tucked beneath your liver — the gallbladder. Yet, for many individuals silently battling unexplained weight gain, the gallbladder may not just be involved; it might be the mastermind.
The question “can gallbladder issues cause weight gain?” isn’t just a curiosity anymore; it’s a growing concern among patients and doctors alike. With more people undergoing gallbladder removal surgeries or living with gallstones, it’s time to unpack this overlooked link — and the biology, pathology, and metabolic consequences behind it.
And if you’re looking for expert intervention, don’t worry — we’ll also guide you to consult a Gallbladder Surgeon in Delhi, where advanced treatment and surgical options are available.
Understanding Gallbladder
Before blaming the gallbladder for your growing waistline, let’s first understand what exactly it does — and what happens when it doesn’t.
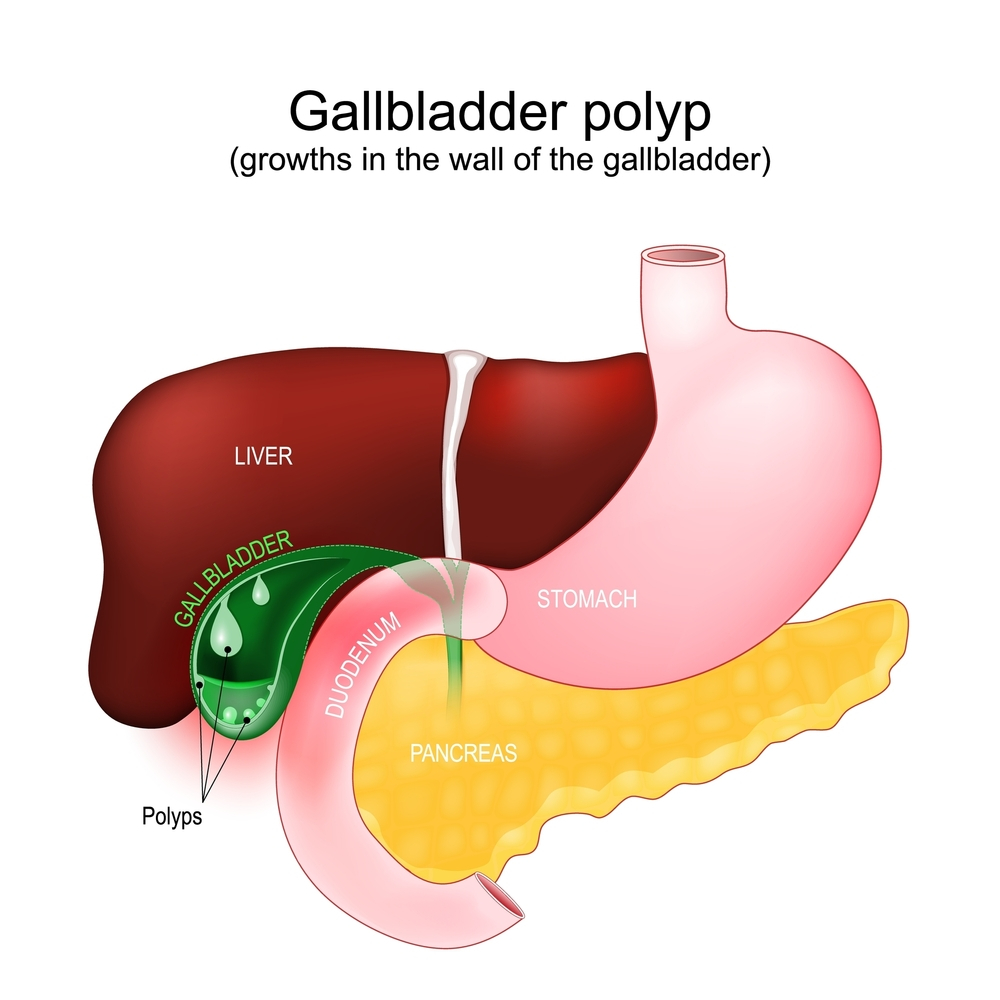
The gallbladder is a small, pouch-like organ located under the liver. Its primary function? To store and concentrate bile, a digestive fluid produced by the liver that helps break down fats into fatty acids, which are easier to absorb in the intestine.
Here’s how the gallbladder normally works:
- You eat a meal, especially one rich in fats.
- Your body signals the gallbladder to contract.
- The gallbladder releases bile into the small intestine.
- Bile emulsifies fats, aiding their digestion and absorption.
So where does weight gain come in?
When the gallbladder fails to function properly — due to inflammation (cholecystitis), infection, poor bile motility, or gallstones (small stones formed from bile components) — fat digestion slows down. And when fats aren’t broken down efficiently, multiple things happen:
- The body struggles to absorb fat-soluble vitamins (A, D, E, K), leading to fatigue and metabolic slowdown.
- Incomplete digestion can cause bloating, sluggish bowel movements, and nutrient imbalances.
- The body, sensing fat malabsorption, may overproduce insulin and store more fat — leading to gradual weight gain.
What are Gallstones?
Let’s clear the smoke: Gallstones are not just little pebbles chilling inside your gallbladder. They are metabolically active saboteurs that can silently disrupt digestion, hormone regulation, and — you guessed it — weight control.
So, What Exactly are Gallstones?
Gallstones (or cholelithiasis) are solid deposits that form from bile components — primarily cholesterol, bilirubin, and bile salts. These stones can range from the size of a grain of sand to that of a golf ball.
There are two main types:
- Cholesterol gallstones (the most common) – composed mainly of undissolved cholesterol.
- Pigment gallstones – made of bilirubin, often linked to liver disease.
Why do they Form?
Imagine your bile as a cleaning solution. When it’s too concentrated or sluggish, or when your gallbladder doesn’t empty properly, that solution crystallizes. Voila — gallstones are born. They can block bile ducts, inflame the gallbladder, and trigger digestive gridlock.
Can Gallbladder Problems Cause Weight Gain? — Mechanisms Explained
The gallbladder isn’t just a passive bile sac. When it malfunctions — either due to sluggish contraction (biliary dyskinesia), infection, or chronic inflammation — the digestive and metabolic sequelae can cascade.
Here’s a breakdown of how a bad gallbladder can cause weight gain:
1. Fatty Acid Malabsorption
Without proper bile release, fats (especially long-chain fatty acids) pass through the gut undigested. You might think “great, less fat absorption = weight loss,” right? Wrong.
Instead, the body compensates by:
- Increasing hunger signals, especially cravings for simple carbs and sugars.
- Decreasing fat-soluble vitamin absorption, affecting thyroid function, immunity, and metabolism.
- Slowing intestinal motility, causing constipation and bloating, which masks weight loss.
2. Hormonal Disruption
Bile plays a role in the conversion of thyroid hormones (T4 to T3) — and a sluggish thyroid means sluggish metabolism. Gallbladder dysfunction is thus indirectly linked to hypothyroid-like symptoms including fatigue, dry skin, and weight gain.
Also, bile helps regulate GLP-1 and PYY — gut hormones that signal fullness. A poorly functioning gallbladder means less bile, less GLP-1 activation, and thus delayed satiety.
3. Low-Grade Inflammation
Chronic gallbladder issues can create a state of systemic low-grade inflammation, which promotes insulin resistance — the cornerstone of obesity.
4. Gut Dysbiosis
Bile has antimicrobial properties that help maintain a healthy microbiome. When bile secretion is disrupted, it allows bad bacteria to proliferate. These bacteria:
- Ferment undigested carbs.
- Create inflammatory byproducts.
- Alter metabolism in a way that promotes weight storage, especially around the belly.
5. Sedentary Recovery Post-Surgery
Many patients who undergo gallbladder removal become less active during the recovery phase. Combine that with digestive upset and appetite changes, and you have a recipe for post-cholecystectomy weight gain.
Thus, while your gallbladder weighs a mere 60-80 grams, a bad gallbladder can cause weight gain that’s several kilos heavy — physically and emotionally.
Weight Gain After Gallbladder Removal: Why It Happens and Who’s at Risk
Picture this: you have finally rid yourself of those mutinous gallstones. The laparoscopic instruments have been packed away, the anaesthetist has wished you good luck, and Dr. Pawanindra Lal tells you that life will soon be back to normal. Fast-forward a few months and your belt buckle is migrating in the wrong direction. You step on the scale, and the digits glare at you with the smugness of a credit-card bill after a holiday binge.
Why does an operation that removes an organ associated with fat digestion so often coincide with gaining fat?
1. Bile No Longer Arrives “On Demand”
In a healthy body, the gallbladder works like a well-timed irrigation valve: it waits until a fatty meal arrives, then delivers a concentrated spurt of bile to emulsify those lipids. Once the reservoir is gone, bile trickles continuously from the liver into the intestine, regardless of whether you are sipping green tea or devouring butter chicken. The result is sub-optimal fat breakdown at mealtimes and a chronic, low-level irritation of the gut in between.
2 Compensatory Carb Cravings
Poorly digested fat leaves you feeling unsatisfied even after adequate calories. The body, ever practical, demands fast energy: enter refined carbohydrates. Post-cholecystectomy patients frequently report new-found cravings for bread, sweets, or rice — precisely the foods that spike insulin and store fat. Hence the search‐friendly lament, “weight gain after gallbladder removal.”
3 Microbiome Mayhem
Bile acids double as an antibacterial detergent. When the delivery rhythm is disrupted, so is the balance of gut flora. Opportunistic bacteria feast, beneficial species shrink, and metabolic signalling goes haywire. Studies link this gut dysbiosis to greater visceral fat and insulin resistance.
4 Hormonal Ripple Effects
Bile acids help convert inactive thyroid hormone (T4) to its metabolically active sibling (T3). Remove the bile reservoir and you often blunt that conversion. Subclinical hypothyroid symptoms (fatigue, lethargy, creeping weight) emerge, even if blood tests hover “within normal limits.”
5 The Sedentary Recovery Trap
Yes, laparoscopic surgery is minimally invasive, but postoperative discomfort still nudges patients toward the couch. Couple that inactivity with the dietary confusion that follows surgery, and kilojoules in exceed kilojoules out.
Who’s Most at Risk?
- Women over 40 — already navigating hormonal shifts that favour fat storage.
- Patients with insulin resistance or metabolic syndrome pre-surgery.
- Those given vague dietary advice (“Just eat what agrees with you”) rather than a structured re-feeding plan.
- Individuals with pre-existing gut disorders such as IBS, where microbiome stability is already fragile.
5 Reasons for Weight Gain After Gallbladder Removal
Weight gain after gallbladder surgery isn’t a myth or a rare side effect — it’s a documented and surprisingly common experience. While every individual’s body responds differently to the absence of a gallbladder, certain physiological patterns appear again and again. These patterns don’t just explain why weight gain happens, but also what you can do to understand and manage it.
Here are five medically recognized reasons for weight gain after gallbladder removal, each of which plays a distinct role in altering how the body processes food, stores fat, and manages metabolism.
1. Continuous, Diluted Bile Flow
The gallbladder’s job was not just to store bile but to release it in concentrated bursts when your body needed it most — during meals, especially those containing fat. After gallbladder removal, bile no longer follows that intelligent timing. Instead, it flows in a constant, weak stream from the liver into the small intestine, even when there’s no food to digest.
This results in suboptimal fat digestion, especially for meals rich in healthy fats like nuts, seeds, avocados, or dairy. Incomplete digestion leads to discomfort, bloating, and the body’s attempt to “solve the problem” by increasing cravings for easily digestible carbs. Over time, this dietary shift encourages insulin spikes, fat storage, and weight gain — particularly in the abdominal region.
2. Impaired Satiety Signals
Bile acids aren’t just passive emulsifiers — they’re key players in gut-brain communication. They stimulate the release of hormones like GLP-1 and PYY, which tell your brain when you’re full. With the gallbladder gone and bile constantly leaking in, this regulatory feedback becomes sluggish.
As a result, you may eat a full meal yet still feel hungry soon after. This is not a matter of willpower — it’s biochemical confusion. Overeating becomes a natural consequence of a body that no longer “feels” full at the right time, leading to gradual but persistent weight gain.
3. Disrupted Gut Flora and Metabolic Shift
When bile flows consistently rather than in coordinated bursts, it disrupts the delicate balance of bacteria in the intestines. The gut microbiome shifts toward species that favor fermentation of carbohydrates and enhanced energy extraction from food. In other words, the same plate of food now yields more calories than it would have before your surgery.
This phenomenon, known as “microbiome-driven obesity,” is gaining ground in research circles. These bacterial shifts not only increase caloric absorption but also create a low-grade inflammatory environment in the gut — one that promotes fat storage, insulin resistance, and metabolic slowdown.
4. Altered Thyroid Function and Slower Metabolism
The absence of a gallbladder can subtly interfere with thyroid hormone conversion, particularly the activation of T3, the hormone responsible for keeping your metabolism humming. Without the gallbladder’s bile-regulating effect, this conversion can become inefficient.
The symptoms are classic and often mistaken for aging or “post-surgery fatigue”: low energy, cold hands and feet, mood swings, and weight gain — even on a modest diet. Many patients report difficulty losing weight even with calorie restriction, reflecting the underlying hormonal stagnation caused by impaired bile dynamics.
5. Post-Surgery Inactivity and Stress Response
Let’s not overlook the most human of factors: recovery. Even minimally invasive laparoscopic surgery requires rest. Most patients reduce physical activity significantly in the weeks following gallbladder removal. Exercise routines are disrupted, and for some, not fully resumed.
This physical inactivity is compounded by surgical stress, disrupted sleep, and dietary confusion. All of these factors elevate cortisol — the body’s primary stress hormone — which is strongly associated with fat accumulation, particularly visceral fat around the midsection. Cortisol also encourages cravings for comfort foods, further feeding the cycle of weight gain.
Strategies to Prevent Gallbladder Weight Gain
The good news is that weight gain after gallbladder removal isn’t a life sentence. Yes, your digestive system has undergone a structural change, and yes, your metabolism may have slowed in response — but with the right interventions, you can restore balance.
This isn’t about crash dieting or doubling down on cardio. It’s about understanding your body’s new digestive rhythm and working with it rather than against it. These strategies are designed not just to help you lose weight, but to improve bile flow, gut health, hormonal balance, and satiety — everything your gallbladder used to support.
1. Reintroduce Fats
One of the biggest mistakes patients make after gallbladder removal is to eliminate fats entirely. While this might feel intuitive — after all, fat digestion is impaired — it actually makes things worse. You need fats to absorb fat-soluble vitamins, regulate hormones, and feel full. What matters is the type and timing of fats.
Start with medium-chain triglycerides (MCTs), such as coconut oil or MCT oil. These don’t require bile for digestion and are quickly absorbed for energy. Over time, you can reintroduce healthy monounsaturated fats like olive oil, avocado, and nuts — but in smaller, more frequent portions.
2. Take Digestive Enzyme
With the gallbladder gone, bile output becomes erratic. To support digestion, many functional medicine practitioners recommend bile salt supplements, particularly those containing ox bile, as well as lipase-rich digestive enzymes. These help break down fats and reduce symptoms like bloating, nausea, or oily stools.
For some patients, this simple addition leads to significant improvement in energy, digestion, and weight regulation.
3. Eat Smaller, More Frequent Meals
Instead of three large meals, shift to five to six smaller meals spread evenly through the day. This eating pattern aligns better with the continuous bile flow that occurs post-surgery. Smaller meals are easier to digest, reduce stress on your gut, and prevent bile from irritating the intestinal lining.
Each meal should contain a balance of protein, fiber, and healthy fats — even if the fat portion is modest. This helps keep your blood sugar stable, reduces cravings, and improves insulin sensitivity.
4. Prioritize Gut Health
Since your microbiome has likely shifted post-surgery, restoring gut flora is a top priority. Introduce probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi, or consider a high-quality probiotic supplement with strains like Lactobacillus and Bifidobacterium.
Equally important is soluble fiber, found in oats, chia seeds, flaxseeds, lentils, and apples. Fiber acts as food for good bacteria, supports bowel regularity, and slows the absorption of sugars — helping you manage your weight and blood glucose more effectively.
5. Support Your Liver and Hormonal Health
With the gallbladder gone, your liver becomes the frontline warrior for bile production. Support it with nutrients like choline (found in eggs), milk thistle (a known hepatoprotective herb), and foods rich in sulfur like garlic and onions. Hydration is also essential — water helps maintain bile viscosity and flow.
For hormonal health, ensure you’re getting adequate vitamin D, magnesium, and iodine — all crucial for thyroid function, which directly influences metabolism.
Experience Advanced Gallbladder Surgery With Dr. Pawanindra Lal!
Book An AppointmentConclusion
Yes, weight gain is complex. It’s never caused by one single organ, one bite of chocolate, or one skipped workout. But to dismiss the gallbladder’s role in digestion, hormonal regulation, and fat metabolism would be a costly oversight. As we’ve seen, can gallbladder issues cause weight gain? — absolutely. And the evidence isn’t just anecdotal; it’s physiological, hormonal, and microbiological.
Whether you’re battling unexplained weight gain, living with gallstones, or struggling to manage your health after gallbladder removal, the path forward begins with awareness. It’s not just about eating less or moving more — it’s about understanding what your body is now trying to adapt to without a gallbladder.
Don’t ignore the signs. That bloating, fatigue, and stubborn belly fat might be more than lifestyle choices gone wrong — they could be your body’s way of saying it’s missing a key piece of its digestive puzzle.
Frequently Asked Questions
1. Can gallbladder issues cause weight gain?
Yes, gallbladder issues can contribute to weight gain through impaired fat digestion, hormonal imbalances, and disrupted bile flow. A dysfunctional gallbladder often leads to fat malabsorption, carb cravings, insulin resistance, and slowed metabolism — all of which can result in gradual weight gain.
2. Can gallstones make you gain weight?
Yes, gallstones can lead to dietary imbalances, poor digestion, and increased cravings — especially for fast-acting carbohydrates. Over time, this results in weight gain, particularly if combined with other factors like sedentary lifestyle or metabolic dysfunction.
3. How much does a gallbladder weigh?
An average gallbladder weighs around 60–80 grams when empty and can hold about 50 milliliters of bile. Though it’s a small organ, its metabolic impact is disproportionately large — especially when it’s removed or dysfunctional.
4. What are the 5 reasons for weight gain after gallbladder removal?
Post-surgical weight gain often results from continuous bile flow, hormonal dysregulation, microbiome imbalances, thyroid slowdown, and reduced physical activity. These factors combine to impair metabolism and promote fat storage, especially when not managed proactively.
5. Is it hard to lose weight without a gallbladder?
Losing weight without a gallbladder is certainly possible, but it requires more intentional management. Adjusting your diet, supporting digestion with enzymes or bile salts, and maintaining consistent exercise can help you lose weight sustainably and safely.